Virtual reality (VR) is gaining traction as a promising tool in Neurorehabilitation, offering innovative ways to enhance recovery for individuals with neurological conditions.
Here’s an overview of its potential, applications, and benefits:
The Potential of Virtual Reality in Neurorehabilitation

1. Immersive Environment
- Engagement: VR creates a controlled, immersive environment that can keep patients engaged and motivated during therapy sessions.
- Customization: Environments can be tailored to individual preferences and rehabilitation goals, making therapy more relevant and enjoyable.
2. Realistic Simulations
- Task-Specific Training: Patients can practice real-life tasks, such as walking, reaching, or navigating obstacles, in a safe setting.
- Gradual Difficulty Adjustment: Therapists can easily modify the difficulty level based on the patient’s progress, providing personalized challenges.
3. Motor and Cognitive Rehabilitation
- Motor Skills: VR can facilitate repetitive practice of movements, which is crucial for motor recovery, particularly after strokes or spinal cord injuries.
- Cognitive Training: It can also enhance cognitive functions through tasks that require attention, memory, and problem-solving skills.
4. Enhanced Feedback
- Immediate Feedback: VR systems can provide real-time feedback on performance, allowing patients to understand their progress and areas for improvement.
- Data Tracking: Progress can be quantitatively tracked over time, aiding in goal setting and adjustments in rehabilitation plans.
5. Social Interaction
- Group Therapy: VR can enable group rehabilitation sessions, where patients can interact and motivate each other, reducing feelings of isolation.
- Remote Rehabilitation: Patients can engage in therapy from home, maintaining social connections and therapeutic support.
Applications in Neurorehabilitation
- Stroke Rehabilitation
- VR can help retrain motor skills and coordination after a stroke, simulating activities like walking or grasping objects.
- Traumatic Brain Injury (TBI) Recovery
- It can aid in cognitive and motor rehabilitation by providing tasks challenging physical and cognitive abilities.
- Parkinson’s Disease
- VR can enhance balance and gait training, allowing patients to practice movements in virtual environments.
- Spinal Cord Injury
- VR exoskeletons and games can support motor function recovery, helping individuals practice movement and coordination.
- Cognitive Rehabilitation
- VR can facilitate tasks that enhance memory, attention, and executive function for conditions like dementia or TBI.
Benefits of Using Virtual Reality

Increased Motivation: The engaging nature of VR can make rehabilitation feel more like a game than a chore.
- Enhanced Learning: Repeated exposure to tasks in a safe environment can help solidify learning and skill acquisition.
- Pain Reduction: Immersion in VR has been shown to reduce perceived pain during rehabilitation exercises.
- Accessibility: VR can be used in a variety of settings, making it easier for patients to access therapy.
Challenges and Considerations
- Cost and Accessibility: The technology can be expensive, and access may be limited in certain regions or healthcare systems.
- Individual Suitability: Not all patients may respond positively to VR; some may experience motion sickness or find the technology overwhelming.
- Need for Professional Guidance: Effective implementation requires trained professionals to guide therapy and ensure patient safety.
Other technologies used in Neurorehabilitation are
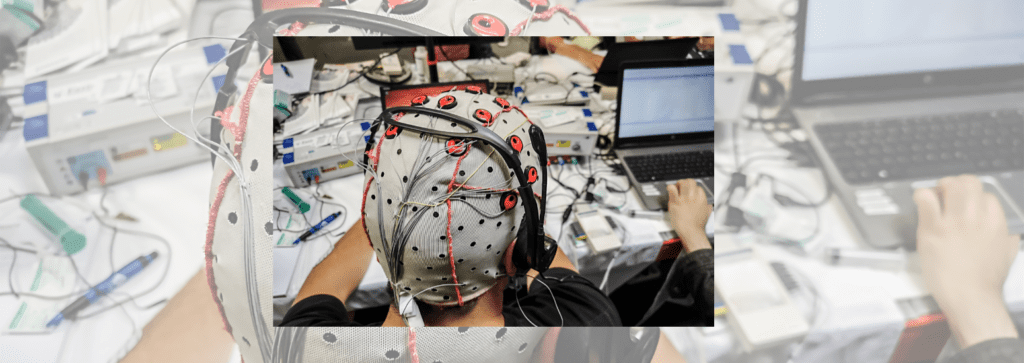
- Brain-computer interfaces (BCIs) – These are revolutionary technologies that enable direct communication between the brain and external devices. They hold significant potential for various applications, particularly in Neurorehabilitation, assistive technology, and even gaming.
A BCI translates brain signals into commands that can control external devices, allowing individuals to interact with computers, prosthetics, or other technology using only their brain activity. This is particularly valuable for individuals with disabilities or neurological disorders.
Below is a comprehensive overview of BCIs, including their components, types, applications, and challenges.
Components of BCIs
- Signal Acquisition:
- Electroencephalography (EEG): Non-invasive method that measures electrical activity on the scalp.
- Intracranial Electrodes: Invasive method that involves implanting electrodes directly in the brain for more precise readings.
- Functional Near-Infrared Spectroscopy: Measures brain activity through hemodynamic responses.
- Signal Processing:
- Algorithms analyze brain signals to identify patterns and translate them into meaningful commands.
- Output Device:
- The device controlled by the BCI, such as a computer cursor, robotic arm, or even a wheelchair.
- User Interface:
- Software that facilitates interaction between the user and the output device.
Types of Brain-Computer Interfaces
- Active BCIs:
- Require the user to actively think about a task (e.g., moving a cursor) to generate specific brain signals.
- Passive BCIs:
- Monitor brain activity without requiring active thought; used for applications like emotional state monitoring.
- Invasive BCIs:
- Involve surgical implantation of electrodes; provide high-resolution data but carry surgical risks.
- Non-Invasive BCIs:
- Use external sensors (e.g., EEG caps); safer but often less precise than invasive methods.
Applications of Brain-Computer Interfaces
- Neurorehabilitation:
- BCIs can assist in the rehabilitation of stroke patients by enabling them to control virtual avatars or robotic limbs, promoting motor learning and recovery.
- Assistive Technology:
- BCIs enable individuals with severe disabilities to control computers, communication devices, or prosthetics, enhancing independence.
- Gaming and Entertainment:
- BCIs are being explored for immersive gaming experiences, allowing players to control games with their thoughts.
- Mental Health Monitoring:
- Passive BCIs can monitor brain activity for signs of stress, anxiety, or depression, providing insights for therapeutic interventions.
- Research:
- BCIs are valuable tools in neuroscience research, helping to study brain function and neural mechanisms.
Challenges and Considerations
- Technical Limitations:
- Current BCIs may struggle with accuracy, latency, and signal noise, which can hinder user experience.
- User Training:
- Users often require training to effectively use BCIs, which can be time-consuming and may vary in success.
- Ethical Concerns:
- Issues related to privacy, consent, and potential misuse of brain data are significant considerations.
- Accessibility and Cost:
- High costs and technical complexity can limit widespread adoption and availability.
- Regulatory Challenges:
- Navigating regulatory frameworks for medical devices can be complex and time-consuming.
Future Directions
- Advancements in Technology:
- Improving signal acquisition methods, processing algorithms, and user interfaces to enhance performance and usability.
- Integration with Other Technologies:
- Combining BCIs with virtual reality (VR) or artificial intelligence (AI) could expand their applications and effectiveness.
- Clinical Trials:
- Continued research and trials to validate BCI applications in real-world settings and refine their designs.
Brain-computer interfaces represent a fascinating frontier in technology, with the potential to transform lives, particularly for individuals with disabilities. As research and technology continue to advance, BCIs could become increasingly effective and accessible, paving the way for new forms of interaction and rehabilitation.
Robotic Exoskeletons
Robotic exoskeletons are wearable devices designed to augment, assist, or enhance human movement. Robotic exoskeletons are a promising technology with the potential to revolutionize rehabilitation, assistive technology, and industrial applications. As advancements continue, these devices could become more effective, accessible, and integrated into everyday life, providing significant benefits to users.
Electrical Stimulation
Electrical stimulation is a therapeutic technique that uses electrical currents to stimulate nerves and muscles for various medical and rehabilitation purposes. This method is widely used in physical therapy, pain management, and neuromuscular re-education. As with any medical treatment, it’s essential to consult with a healthcare professional to determine the most appropriate type and approach based on individual needs and conditions.
Conclusion
Virtual reality holds significant potential for enhancing Neurorehabilitation, offering innovative ways to engage patients and improve outcomes. As technology advances and becomes more accessible, its integration into rehabilitation programs could transform traditional approaches and foster more effective recovery pathways.the quality of life for individuals with autism and their families.



