Delving into Different Headache Types and Their Neurological Connections
Headaches can be categorized into primary types, like tension headaches, migraines, and cluster headaches, each with distinct neurological mechanisms. Tension headaches are often linked to muscle tension and stress, while migraines involve neurovascular changes and can be triggered by various factors. Cluster headaches, characterized by severe pain in cyclical patterns, are believed to involve hypothalamic dysfunction and autonomic nervous system activation.
Different Types of Headaches
Migraine
Migraine is a neurological condition characterized by recurrent headaches that can vary in intensity, frequency, and duration. It often includes a range of symptoms beyond just head pain.
Symptoms of Migraine
- Headache:
Typically, unilateral (one side of the head), throbbing or pulsating in nature, and moderate to severe in intensity.
- Aura:
Some individuals experience neurological symptoms before or during the headache, such as visual disturbances (flashes of light, zigzag patterns), sensory changes (numbness or tingling), or speech difficulties.
- Nausea and Vomiting:
Many people experience gastrointestinal symptoms, including nausea and vomiting.
- Sensitivity to Light and Sound:
Increased sensitivity to light and sound is common during an attack.
- Fatigue and Mood Changes:
Fatigue, irritability, or a feeling of euphoria can occur before or after a migraine episode.
Diagnosis of Migraine
- Clinical History:
A detailed medical history, including headache frequency, duration, intensity, and associated symptoms, is essential for diagnosis.
- Diagnostic Criteria:
Diagnosis is often based on the International Classification of Headache Disorders (ICHD) criteria, which include specific features and patterns of headache episodes.
- Exclusion of Other Conditions:
Healthcare providers may perform tests (e.g., MRI or CT scans) to rule out other potential causes of headaches, particularly if the presentation is atypical.
- Headache Diary:
Keeping a headache diary can help track frequency, duration, triggers, and symptoms, aiding in diagnosis and treatment planning.
A thorough evaluation by a healthcare professional is crucial for an accurate diagnosis and effective management of migraines.
Treatment of Migraine
Migraine treatment typically involves a combination of acute (abortive) therapies to relieve symptoms during an attack and preventive (prophylactic) treatments to reduce the frequency and severity of episodes.
Here’s an overview of both approaches:
Acute Treatment
- Over-the-Counter Medications:
- NSAIDs: Ibuprofen, naproxen, or aspirin can help relieve mild to moderate migraine pain.
- Acetaminophen: Effective for some individuals, particularly when combined with caffeine.
- Prescription Medications:
- Triptans: Medications like sumatriptan, rizatriptan, and eletriptan specifically target migraine symptoms by constricting blood vessels and alleviating pain.
- Ergots: Less commonly used, medications like ergotamine can help in certain cases, especially if taken early.
- Anti-Nausea Medications:
Medications such as metoclopramide or prochlorperazine can help manage nausea and vomiting associated with migraines.
- CGRP Inhibitors:
Newer medications, such as ubrogepant and rimegepant, target the calcitonin gene-related peptide (CGRP) involved in migraine attacks.
Preventive Treatment
- Medications:
- Beta-Blockers: Propranolol and metoprolol are commonly prescribed to reduce migraine frequency.
- Antidepressants: Certain antidepressants, like amitriptyline, can be effective in preventing migraines.
- Anticonvulsants: Medications such as topiramate and valproate can also serve as preventive treatments.
- CGRP Monoclonal Antibodies: Medications like erenumab, fremanezumab, and galcanezumab are newer options specifically designed to prevent migraines.
- Lifestyle Modifications:
- Trigger Management: Identifying and avoiding personal migraine triggers (e.g., certain foods, stress, sleep patterns) can significantly reduce attacks.
- Regular Exercise: Moderate, consistent physical activity can help reduce the frequency of migraines.
- Stress Management: Techniques such as mindfulness, meditation, and cognitive behavioral therapy can be beneficial.
- Alternative Therapies:
- Acupuncture: Some individuals find relief through acupuncture treatments.
- Biofeedback: This technique teaches individuals to control physiological functions, which may help reduce headache frequency.
Effective migraine treatment often requires a personalized approach, combining medications, lifestyle changes, and alternative therapies. Consulting with a healthcare provider is essential for developing a comprehensive management plan tailored to individual needs and preferences.
Cluster headaches
Cluster headaches are a type of primary headache disorder characterized by severe, unilateral pain that occurs in cyclical patterns or clusters. They are often described as one of the most painful types of headaches.
Symptoms of Cluster Headaches
- Severe Pain:
Intense, stabbing pain usually located around one eye or one side of the head, often described as excruciating.
- Duration:
Attacks typically last from 15 minutes to three hours and can occur multiple times a day during a cluster period.
- Timing:
Headaches often occur at the same time each day, frequently during sleep or in the early morning.
- Autonomic Symptoms:
Associated symptoms may include redness or tearing of the eye, nasal congestion or runny nose, drooping of the eyelid, and swelling around the eye on the affected side.
- Restlessness:
Individuals often exhibit restlessness or agitation during an attack, unable to sit still.
Diagnosis of Cluster Headaches
- Clinical History:
A thorough medical history and description of headache patterns, including duration, frequency, and associated symptoms.
- Physical Examination:
Neurological examination to rule out other conditions and confirm headache type.
- Diagnostic Criteria:
Diagnosis is often based on criteria established by the International Classification of Headache Disorders (ICHD), which requires specific features and patterns of the headache.
- Exclusion of Other Conditions:
Imaging tests (e.g., MRI or CT scans) may be conducted to rule out other potential causes of severe headaches.
Treatment of Cluster Headaches
Acute Treatment…
- Oxygen Therapy:
Inhaling 100% oxygen through a mask for 15-20 minutes can provide rapid relief for many individuals.
- Triptans:
Medications like sumatriptan or zolmitriptan can be effective for aborting an attack, usually administered via injection or nasal spray.
- Ergotamine:
Less commonly used, but can be effective if taken early in the attack.
Preventive Treatment…
Medications:
- Verapamil: A calcium channel blocker that is the first-line preventive treatment for cluster headaches.
- Corticosteroids: Short-term use can help during an acute cluster period to reduce the frequency and severity of attacks.
- Lithium: Sometimes used for chronic cluster headaches, particularly if other treatments are ineffective.
Neuromodulation:
Occipital Nerve Stimulation: A Neuromodulation technique involving implanting a device to stimulate the occipital nerve, providing relief for some patients.
Lifestyle Modifications:
Avoiding known triggers, maintaining a consistent sleep schedule, and managing stress may help reduce the frequency of attacks.
Tension headaches
Tension headaches are the most common type of primary headache, often described as a dull, aching pain that can feel like a tight band around the head. They may be episodic or chronic and are generally less severe than migraines.
Symptoms of Tension Headaches
- Pain Quality:
Mild to moderate, pressing or tightening sensation; often described as a “band-like” pressure around the forehead.
- Location:
Pain is typically bilateral (affecting both sides of the head) and can radiate to the neck, shoulders, or jaw.
- Duration:
Episodes can last from 30 minutes to several days, with some individuals experiencing headaches daily.
- Associated Symptoms:
Unlike migraines, tension headaches are generally not accompanied by nausea or vomiting. Sensitivity to light or sound may be mild.
- Muscle Tension:
Tenderness or tightness in the neck, shoulders, or scalp may accompany the headache.
Diagnosis of Tension Headaches
- Clinical History:
A detailed medical history, including headache frequency, duration, intensity, and associated symptoms.
- Physical Examination:
A neurological examination to rule out other potential causes of headache.
- Diagnostic Criteria:
Diagnosis often follows the International Classification of Headache Disorders (ICHD) criteria, which classify headaches based on specific features.
- Exclusion of Other Conditions:
Imaging tests (e.g., MRI or CT scans) may be used if the headache presentation is atypical or if there are concerning neurological signs.
Treatment of Tension Headaches
Acute Treatment
Over-the-Counter Medications:
- NSAIDs: Ibuprofen, naproxen, or aspirin can help relieve pain.
- Acetaminophen: Another option for mild to moderate pain relief.
Prescription Medications:
If OTC medications are ineffective, a healthcare provider may prescribe stronger pain relievers.
Subarachnoid Hemorrhage
Subarachnoid Hemorrhage is a serious medical condition characterized by bleeding into the subarachnoid space, the area between the brain and the tissues covering it. This condition often results from a ruptured aneurysm or head injury and can lead to significant complications.
Symptoms of Subarachnoid Hemorrhage
- Sudden, Severe Headache:
Often described as a “thunderclap” or the worst headache of the person’s life, it occurs suddenly and is intense.
- Nausea and Vomiting:
Many individuals experience nausea and vomiting as a response to the severe pain.
- Neck Stiffness:
Stiffness and pain in the neck due to irritation of the meninges (the membranes surrounding the brain).
- Photophobia:
Sensitivity to light, which can accompany the headache.
- Altered Consciousness:
Changes in consciousness, confusion, or even loss of consciousness may occur.
- Seizures:
Some individuals may experience seizures due to the irritation of the brain.
Diagnosis of Subarachnoid Hemorrhage
- Clinical Evaluation:
A detailed medical history and physical examination, focusing on neurological status.
- Imaging Studies:
- CT Scan: A non-contrast CT scan of the head is often the first step and can quickly identify blood in the subarachnoid space.
- MRI: This may be used for further evaluation, although it is less common in acute settings.
- Lumbar Puncture:
If CT is inconclusive but SAH is suspected, a lumbar puncture (spinal tap) may be performed to check for blood in the cerebrospinal fluid (CSF).
- Angiography:
Cerebral Angiography: This imaging test can identify any vascular abnormalities, such as aneurysms or arteriovenous malformations (AVMs).
Treatment of Subarachnoid Hemorrhage
- Emergency Care:
Immediate medical attention is critical. Stabilization of vital signs and prevention of complications are priorities.
- Surgical Intervention:
- Aneurysm Clipping: If the Hemorrhage is due to a ruptured aneurysm, a neurosurgeon may perform surgery to clip the aneurysm and prevent further bleeding.
- Endovascular Coiling: A less invasive option where coils are inserted into the aneurysm via catheter to promote clotting and seal off the aneurysm.
- Supportive Care:
Management of pain, nausea, and other symptoms, along with close monitoring for complications such as rebleeding, vasospasm (narrowing of blood vessels), and hydrocephalus (accumulation of CSF).
- Medications:
Calcium Channel Blockers (e.g., nimodipine) may be used to prevent vasospasm and improve outcomes.
- Rehabilitation:
Following stabilization, individuals may require rehabilitation services to address neurological deficits and improve function.
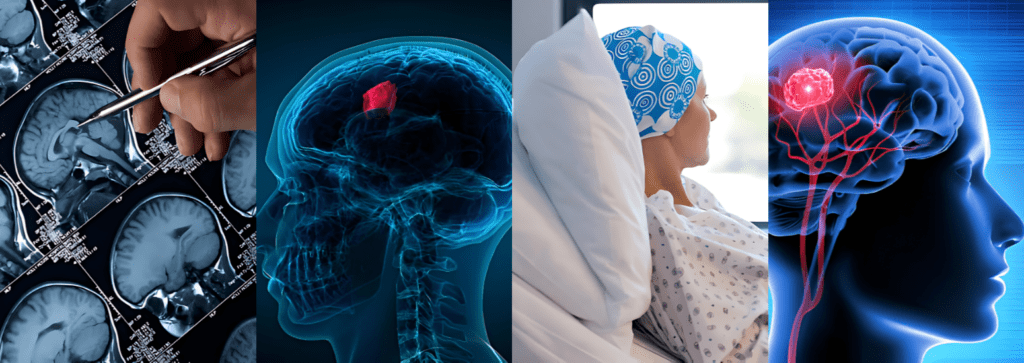
Brain tumor –
A brain tumor is an abnormal growth of cells within the brain. Tumors can be benign (non-cancerous) or malignant (cancerous) and can originate in the brain (primary tumors) or spread from other parts of the body (metastatic tumors).
Symptoms of Brain Tumor
Symptoms can vary widely based on the size of the tumor, type, and location but commonly include:
- Headaches:
Persistent or worsening headaches, often worse in the morning or during the night.
- Nausea and Vomiting:
Frequent nausea and vomiting, especially if associated with headaches.
- Cognitive Changes:
Memory problems, difficulty concentrating, or confusion.
- Neurological Deficits:
Weakness or numbness in limbs, difficulty with coordination or balance, and changes in speech.
- Seizures:
New-onset seizures, which may be focal or generalized.
- Visual or Auditory Disturbances:
Blurred vision, double vision, or hearing problems.
- Personality Changes:
Changes in mood or personality, including increased irritability or emotional instability.
Diagnosis of Brain Tumor
- Clinical Evaluation:
A thorough medical history and physical examination focusing on neurological function.
- Imaging Studies:
- MRI (Magnetic Resonance Imaging): The preferred method for visualizing brain tumors, providing detailed images of brain structures.
- CT Scan (Computed Tomography): Often used in emergency settings to assess the brain quickly.
- Biopsy:
A definitive diagnosis often requires a tissue sample obtained through a needle biopsy or surgical resection to determine tumor type and grade.
- Neuropsychological Testing:
Assessing cognitive function can help determine the impact of the tumor on brain function.
Treatment of Brain Tumor
- Surgery:
Surgical resection is often the first line of treatment, aimed at removing as much of the tumor as possible. This may also provide a tissue sample for diagnosis.
- Radiation Therapy:
Often used after surgery to target remaining tumor cells or as a primary treatment for inoperable tumors. Techniques include external beam radiation and stereotactic radiosurgery.
- Chemotherapy:
Medications may be used to target cancer cells, particularly for malignant tumors. The choice of chemotherapy agents depends on the tumor type.
- Targeted Therapy:
For specific types of tumors, targeted therapies may be employed that focus on particular cellular mechanisms involved in tumor growth.
- Supportive Care:
Management of symptoms such as headaches, nausea, and seizures, as well as physical, occupational, and speech therapy to address functional deficits.
- Clinical Trials:
Participation in clinical trials may be an option for accessing new and experimental treatments.
Neurorehabilitation
Neurorehabilitation plays a crucial role in managing different types of headaches by addressing physical and psychological factors. Techniques such as cognitive behavioral therapy, biofeedback, and physical therapy can help reduce tension and improve coping strategies, particularly for tension and migraine headaches.
For cluster headaches, supportive counseling and pain management strategies enhance quality of life. In chronic daily headaches, a comprehensive, multimodal approach tailored to individual needs is essential for effective management and improved function.
A tailored, multidisciplinary approach can significantly enhance patients’ quality of life and overall functioning.



