Understanding Neurorehabilitation
Neurorehabilitation is a specialized branch of medicine focused on helping individuals recover from neurological conditions and injuries, such as stroke, traumatic brain injury, spinal cord injury, multiple sclerosis, Parkinson’s disease, and other disorders affecting the brain, spinal cord, or nervous system. The goal of Neurorehabilitation is to maximize functional recovery, independence, and quality of life for patients.
Key Aspects of Neurorehabilitation
1. Multidisciplinary Approach
Neurorehabilitation involves a team of healthcare professionals, including:
- Neurologists: Medical doctors specializing in nervous system disorders.
- Physiotherapists: Focus on restoring physical function and mobility.
- Occupational Therapists: Help patients regain daily living skills like dressing, cooking, and bathing.
- Speech and Language Therapists: Assist with communication and swallowing difficulties.
- Rehabilitation Nurses: Provide specialized care for patients recovering from neurological injuries.
2. Recovery of Motor Function
- Physical Therapy: This includes exercises to improve balance, strength, coordination, and movement. Techniques such as gait training and task-specific practice help patients regain mobility.
- Robotic-Assisted Rehabilitation: Devices like exoskeletons and robotic arms are used to aid motor recovery, especially in individuals with paralysis or severe motor impairments.
3. Cognitive Rehabilitation
- Cognitive Training: Patients undergo exercises to improve memory, attention, problem-solving, and executive functions. This is particularly important for those who have experienced traumatic brain injuries or strokes affecting cognitive abilities.
- Neurofeedback: A technique that uses real-time monitoring of brain activity to help patients train their brains to function more effectively.
4. Speech and Language Rehabilitation
- Aphasia Therapy: This helps patients recover language skills following a stroke or brain injury. It involves exercises to improve word retrieval, speech production, and comprehension.
- Swallowing Therapy (Dysphagia Treatment): Involves exercises and techniques to help patients regain the ability to swallow safely.
5. Psychosocial Rehabilitation
- Emotional and Behavioral Therapy: Many patients experience emotional challenges, such as depression, anxiety, or personality changes after a neurological injury. Therapy focuses on coping strategies and emotional regulation.
- Family Counseling: Neurorehabilitation often involves the patient’s family, providing them with guidance on how to support recovery and manage the psychological impact of a loved one’s condition.
6. Technological Innovations
- Virtual Reality (VR): VR is increasingly being used for immersive rehabilitation experiences that improve motor and cognitive recovery. It creates engaging, real-world simulations to practice daily tasks.
- Brain-Computer Interfaces (BCIs): BCIs allow patients to control devices with their brain activity, offering new avenues for communication and movement, especially in those with severe paralysis.
- Transcranial Magnetic Stimulation (TMS): A non-invasive treatment that uses magnetic fields to stimulate specific areas of the brain, promoting neural repair and improving motor or cognitive functions.
7. Neuroplasticity
Neurorehabilitation capitalizes on the brain’s ability to reorganize itself—known as neuroplasticity. By repeatedly practicing tasks, the brain can form new neural connections, allowing patients to regain lost functions or compensate for damaged areas.
8. Community Reintegration
Rehabilitation is not just about regaining physical or cognitive abilities, but also about reintegrating into everyday life. This involves:
- Social skills training: Helping patients reconnect with friends and participate in community activities.
- Vocational rehabilitation: Supporting patients in returning to work or finding new
- employment opportunities if needed.
Common Conditions Treated in Neurorehabilitation
- Stroke: One of the most common reasons for Neurorehabilitation. Therapy focuses on recovering motor, language, and cognitive functions.
- Traumatic Brain Injury (TBI): This often requires long-term rehabilitation for issues such as memory loss, motor impairment, and emotional disturbances.
- Spinal Cord Injuries: Therapy is directed at improving mobility, managing pain, and maximizing independence with adaptive devices.
- Multiple Sclerosis (MS): Neurorehabilitation helps manage symptoms, prevent complications, and improve quality of life.
- Parkinson’s Disease: Rehabilitation focuses on maintaining mobility, balance, and coordination, as well as speech therapy.
Goals of Neurorehabilitation

The primary objectives of Neurorehabilitation include:
- Maximizing independence: Helping patients regain autonomy in daily activities.
- Restoring function: Encouraging recovery of lost motor, cognitive, and communication skills.
- Improving quality of life: Reducing pain, discomfort, and psychological stress.
- Preventing complications: Managing secondary issues like pressure ulcers, muscle atrophy, or contractures.
Neurorehabilitation is a dynamic and evolving field, and with advances in technology and neuroscience, the potential for recovery and improved outcomes continues to grow.
Main traditional Neurorehabilitation Approaches:
Traditional Neurorehabilitation approaches focus on restoring function and promoting recovery after neurological injuries through established therapies that have been used for decades. These approaches remain foundational in Neurorehabilitation care. They primarily target motor, cognitive, speech, and emotional recovery.
Physical Therapy
Physical therapy is one of the most widely used traditional approaches in Neurorehabilitation, primarily aimed at improving motor function, strength, balance, and mobility.
- Therapeutic Exercises: Exercises designed to strengthen muscles, improve coordination, and restore movement patterns. These exercises are customized based on the patient’s needs.
- Balance and Coordination Exercises: Focus on improving stability and preventing falls, particularly important in patients with conditions like Parkinson’s disease or cerebellar dysfunction.
Occupational Therapy
Occupational therapy aims to help individuals regain the ability to perform daily activities (also called Activities of Daily Living) and return to meaningful occupations, whether at home or work.
- Fine Motor Skills Rehabilitation: Exercises to improve hand-eye coordination, dexterity, and hand strength, often lost after a stroke or brain injury.
- Energy Conservation Techniques: Strategies to manage fatigue, especially for patients with neurological conditions like multiple sclerosis.
Speech and Language Therapy
This approach addresses communication disorders and swallowing difficulties (dysphagia) resulting from neurological damage.
- Aphasia Therapy: Exercises to improve language skills for patients who have difficulty understanding or producing speech due to brain injuries like stroke.
- Speech Articulation Therapy: Techniques to enhance clarity of speech for individuals with slurred or impaired speech (dysarthria) resulting from motor control issues.
- Voice Therapy: For patients with vocal quality issues, such as those caused by Parkinson’s disease, therapy focuses on improving vocal strength and control.
- Swallowing Therapy (Dysphagia): Techniques to help patients regain safe swallowing abilities, often using exercises to strengthen throat muscles or alter eating strategies to prevent choking.

Cognitive Rehabilitation Therapy
Cognitive rehabilitation focuses on restoring or compensating for impaired cognitive functions such as memory, attention, problem-solving, and executive functioning.
Neuropsychological Counseling
Many neurological injuries can result in emotional or behavioral changes. Neuropsychological counseling addresses these psychological effects through:
- Cognitive-Behavioral Therapy: Helps patients develop coping strategies for emotional challenges like depression, anxiety, or frustration, which often arise after brain injuries or neurological conditions.
- Emotional Support: Counseling provides a space for patients to process feelings about their condition, manage stress, and improve emotional well-being.
- Family Counseling: Traditional Neurorehabilitation often involves working with the patient’s family to help them understand the condition and provide better support.
Manual Therapy and Neurodevelopmental Techniques
Manual therapy focuses on hands-on techniques, particularly for patients with movement impairments. One common method is Neurodevelopmental Treatment
Neurodevelopmental Treatment: A hands-on approach that focuses on normalizing movement patterns in individuals with motor impairments due to stroke or cerebral palsy. It involves guiding patients through movements to retrain the nervous system to move in more functional ways.
Sensory Stimulation
For patients with reduced awareness or sensory impairments (e.g., from a stroke or brain injury), sensory stimulation techniques aim to increase responsiveness to external stimuli.
- Visual and Auditory Stimulation: Using light or sound to elicit a response, especially in comatose or minimally responsive patients.
- Vestibular Stimulation: Techniques to improve balance and coordination by stimulating the inner ear’s balance mechanisms, often through head and body movements.
Traditional Therapies for Emotional and Behavioral Adjustment
- Behavioral Modification: This involves using reinforcement techniques to encourage positive behavior and reduce maladaptive actions, especially important in brain injury patients with behavioral challenges.
- Support Groups and Peer Support: Group therapy and peer support sessions provide emotional support, encouragement, and practical advice from others who have experienced similar challenges.
Emerging Trends in Neurorehabilitation Therapies:

Exoskeletons for mobility…
Exoskeletons are wearable robotic devices designed to assist with mobility and rehabilitation, particularly in individuals with neurological impairments such as spinal cord injuries, stroke, multiple sclerosis, and cerebral palsy. These devices are becoming increasingly important in Neurorehabilitation, providing patients with the opportunity to regain some level of mobility, enhance muscle strength, and improve overall physical health.
Key Benefits of Exoskeletons in Neurorehabilitation
- Restoring Mobility
- Neuroplasticity and Functional Recovery
- Improving Muscle Strength and Endurance
- Enhancing Motivation and Psychological Well-being
- Reducing Secondary Complications
Brain-computer interfaces…
Brain-computer interfaces represent a significant innovation in Neurorehabilitation, offering new ways for individuals with neurological injuries or diseases to regain lost functions. BCIs work by translating brain activity into external commands, allowing users to control devices, software, or even their body movements without relying on muscle activity. This technology is particularly beneficial for patients with severe mobility impairments, such as those with spinal cord injuries, stroke, amyotrophic lateral sclerosis (ALS), or other neuromuscular disorders.
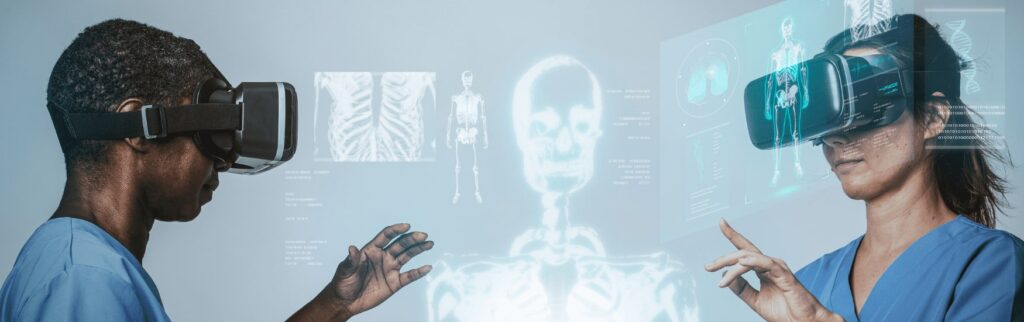
Virtual and augmented reality therapy…
Virtual Reality (VR) and Augmented Reality (AR) are emerging as powerful tools in Neurorehabilitation, offering new and engaging ways to help patients recover from neurological injuries or diseases. These technologies provide immersive environments where patients can safely practice motor and cognitive tasks, receive real-time feedback, and engage in personalized rehabilitation programs.
Deep Brain Stimulation:
Deep Brain Stimulation (DBS) is an advanced therapy that involves the surgical implantation of electrodes in specific brain regions to deliver electrical impulses. It is primarily known for treating movement disorders like Parkinson’s disease, but DBS is also being explored for a range of neurological and psychiatric conditions in the context of Neurorehabilitation. By modulating abnormal neural activity, DBS can help restore functional abilities, improve motor control, and alleviate symptoms of neurological disorders.
How VR and AR Work in Neurorehabilitation Therapies
- Virtual Reality (VR): In VR, patients are fully immersed in a computer-generated 3D environment where they can interact with objects and perform exercises. Through the use of VR headsets or motion-tracking systems, patients can engage in tasks that mimic real-world activities but are customized for their rehabilitation needs.
- Augmented Reality (AR): AR overlays digital information or images onto the real-world environment through devices like smartphones, tablets, or AR glasses. This allows patients to interact with real and virtual elements simultaneously, making rehabilitation exercises more dynamic and engaging.
Future of Neurorehabilitation at PERKESO

The future of Neurorehabilitation at PERKESO (Social Security Organization, Malaysia) holds immense potential for growth, innovation, and improved patient outcomes. By integrating cutting-edge technologies, data-driven strategies, and comprehensive patient care, PERKESO can become a leader in Neurorehabilitation services in the region. Below are key trends and future directions that could shape the future of Neurorehabilitation at PERKESO.
1.Integration of Advanced Technologies
PERKESO is likely to continue incorporating advanced technologies to enhance Neurorehabilitation services:
- Robotics and Exoskeletons
- Virtual Reality (VR) and Augmented Reality
- Brain-Computer Interfaces (BCIs)
2. Personalized Neurorehabilitation Therapies
The future at PERKESO will likely see a shift toward personalized rehabilitation programs tailored to individual patients’ specific needs, capabilities, and recovery goals.
3. Comprehensive Multidisciplinary Care
Neurorehabilitation at PERKESO will continue to prioritize a multidisciplinary approach involving neurologists, physiotherapists, occupational therapists, speech therapists, psychologists, and other healthcare professionals.
4. Neuroplasticity-Enhancing Therapies
Leveraging the brain’s ability to rewire itself (neuroplasticity) is a key goal in Neurorehabilitation. Future therapies at PERKESO will focus on boosting neuroplasticity through various means:
5. Expanding Accessibility and Outreach
The future of Neurorehabilitation at PERKESO will involve making rehabilitation services more accessible to people in rural or underserved areas:
- Tele-rehabilitation Networks: By expanding telehealth networks, PERKESO can reach patients who are unable to visit rehabilitation centers regularly. This can be achieved through mobile clinics, teleconsultations, and remote therapy sessions, ensuring that patients receive continuous care no matter their location.
- Community-Based Rehabilitation: Partnering with local healthcare providers and community organizations to deliver community-based rehabilitation programs could increase patient access and engagement. This would involve training local healthcare workers to provide basic rehabilitation services under the guidance of specialized therapists.
6. Research and Innovation
PERKESO will likely become a hub for clinical research and innovation in Neurorehabilitation:
- Collaborative Research: Partnering with universities, research institutions, and healthcare technology companies will allow PERKESO to conduct clinical trials, test new therapies, and contribute to global advancements in Neurorehabilitation.
- Patient-Reported Outcomes and Feedback: By systematically collecting patient feedback and outcomes, PERKESO will continuously refine its rehabilitation programs. This feedback-driven approach will help ensure that therapies remain effective and patient-centered.
Conclusion
The future of Neurorehabilitation at PERKESO is poised to be shaped by technological advancements, personalized care models, and innovative treatment methods. Moreover, focusing on neuroplasticity-enhancing techniques, expanding outreach to underserved communities, and fostering collaborative research will further solidify PERKESO’s role as a leader in Neurorehabilitation.
These innovations will ultimately improve patient outcomes, quality of life, and reintegration into society.



