According to WHO – The World Health Organisation defines paralysis as a central nervous system disorder that results in difficulty or inability to move the upper or lower extremities.
When nerves can’t send signals to muscles, it causes paralysis, making it impossible to move voluntarily. Strokes, spinal cord injuries, and nerve disorders like multiple sclerosis often cause paralysis. Bell’s palsy causes temporary facial paralysis. Paraplegia affects both legs, while quadriplegia affects all limbs.
Understanding the degrees of severity of paralysis is crucial as it guides in providing the right care and support.
Some people may experience temporary paralysis and regain partial or complete movement over time. For instance, Bell’s palsy causes temporary paralysis of the facial muscles. Palsy refers to paralysis accompanied by tremors. Permanent paralysis indicates a loss of muscle control that cannot be reversed.
Paralysis can impact any body part and can be categorised as partial (paresis), where some muscles are controllable but not all, or complete, where there is no control over any muscles. Additionally, paralysis can be classified into two types based on the site of injury in the nervous system: flaccid, where muscles become flabby and shrink, and spastic, where muscles tighten and cause uncontrollable jerks and spasms (spasticity).

What are the conditions that can result in Paralysis?
1. Acute Flaccid Myelitis (AFM)
A rare but serious condition that affects the nervous system, specifically the grey matter of the spinal cord, causing muscles and reflexes to become weak. Symptoms can include sudden onset of arm or leg weakness, loss of muscle tone and reflexes, and facial weakness. It can be caused by various viral infections.
2. Amyotrophic Lateral Sclerosis (ALS)
A progressive neurodegenerative disease that affects nerve cells in the brain and spinal cord. It leads to the gradual degeneration and death of motor neurons, resulting in muscle weakness, twitching, and eventually, complete loss of voluntary muscle control. ALS is also known as Lou Gehrig’s disease.
3. Arteriovenous Malformation (AVM)
An abnormal tangle of blood vessels connecting arteries and veins, which disrupts normal blood flow and oxygen circulation. AVMs can occur in various parts of the body, including the brain and spine, and can lead to serious health issues like bleeding, seizures, and neurological deficits.
4. Brachial Plexus Injury
An injury to the network of nerves that sends signals from the spine to the shoulder, arm, and hand (the brachial plexus). It can result from trauma, inflammation, or birth-related injuries. Symptoms include weakness, loss of feeling, or loss of movement in the shoulder, arm, or hand.
5. Brain Injury
Damage to the brain that can result from trauma (such as a blow to the head), lack of oxygen, or other medical conditions. Brain injuries can be classified as traumatic (Traumatic Brain Injury) or non-traumatic (such as stroke or infection). Symptoms and severity vary widely and can include cognitive, physical, and emotional impairments.
6. Cerebral Palsy (CP)
A group of disorders that affect movement and muscle tone or posture. It is caused by damage that occurs to the immature, developing brain, most often before birth. Symptoms vary but generally include exaggerated reflexes, rigidity or floppiness of the limbs and trunk, abnormal posture, involuntary movements, and unsteady walking.

7. Friedreich’s Ataxia
A rare, inherited disease that causes progressive damage to the nervous system. It leads to symptoms including gait disturbance, speech problems, and heart disease. Friedreich’s Ataxia typically results from a genetic mutation affecting the production of the frataxin protein.
8. Guillain-Barré Syndrome (GBS)
A rare neurological disorder in which the body’s immune system mistakenly attacks the peripheral nerves. Symptoms often start with weakness and tingling in the feet and legs that can spread to the upper body. Severe cases can lead to paralysis. GBS is often triggered by an infection.
9. Leukodystrophies
A group of rare, inherited disorders that affect the white matter of the brain. They involve the growth or development of the myelin sheath, which insulates nerve cells. Symptoms can include loss of motor skills, muscle stiffness, and developmental delays. Each type of leukodystrophy is caused by mutations in different genes.
10. Lyme Disease
An infectious disease caused by the bacterium Borrelia burgdorferi, transmitted to humans through the bite of infected black-legged ticks. Early symptoms include fever, headache, fatigue, and a characteristic skin rash called erythema migrans. If left untreated, the infection can spread to the joints, heart, and nervous system.
11. Multiple Sclerosis (MS)
A chronic autoimmune disease that affects the central nervous system (brain and spinal cord). Multiple Sclerosis involves an abnormal response of the body’s immune system against the myelin sheath, the protective covering of nerve fibres, causing inflammation and damage. This leads to symptoms such as fatigue, walking difficulties, numbness, and muscle weakness.
12. Neurofibromatosis
Neurofibromatosis is a genetic disorder that causes tumours to form on nerve tissue. These tumors can develop anywhere in the nervous system, including the brain, spinal cord, and nerves. There are three types: neurofibromatosis type 1 (NF1), Neurofibromatosis type 2 (NF2), and Schwannomatosis, each with distinct characteristics and symptoms like skin changes, bone deformities, and hearing loss.
13. Post-Polio Syndrome (PPS)

A condition that affects polio survivors years after recovery from an initial acute attack of the poliovirus. It is characterised by new muscle weakness, fatigue, and pain. The cause is believed to be the gradual deterioration of motor neurons initially damaged by the poliovirus.
14. Spina Bifida
A congenital disability where there is incomplete closing of the backbone and membranes around the spinal cord. It is a type of neural tube defect that can result in physical and intellectual disabilities that range from mild to severe, depending on the size and location of the opening in the spine.
15. Spinal Cord Injury (SCI)
Damage to the spinal cord that results in a loss of function, such as mobility or feeling. Causes can include trauma (car accident, gunshot, falls) or disease (polio, spina bifida). Symptoms vary widely depending on the location and severity of the injury but often include paralysis and sensory loss below the level of injury.
16. Spinal Muscular Atrophy (SMA)
A genetic disease affecting the part of the nervous system that controls voluntary muscle movement. It is caused by a mutation in the SMN1 gene. SMA involves the loss of motor neurons and leads to muscle weakness and atrophy. There are several types, ranging from severe (type 1) to milder forms (type 4).
17. Spinal Tumours
Abnormal growths of tissue within or surrounding the spinal cord and spinal column. They can be benign (non-cancerous) or malignant (cancerous). Symptoms often include back pain, neurological problems, and, depending on the location, loss of sensation or motor function.
18. Stroke
A medical condition where poor blood flow to the brain results in cell death is known as Stroke. There are two main types: ischaemic (due to lack of blood flow) and hemorrhagic (due to bleeding). Symptoms can include sudden numbness or weakness, especially on one side of the body, confusion, trouble speaking, and loss of coordination.
19. Transverse Myelitis
A neurological disorder caused by inflammation across both sides of one spinal cord segment. This inflammation can damage the myelin and disrupt the typical responses from the nerves in the spinal cord to the rest of the body. Symptoms include pain, muscle weakness, paralysis, sensory problems, and bladder and bowel dysfunction.
What are therapy plans for paralysis?
1. Assessment and Individualised Plans:
- Creating individualised therapy plans based on a comprehensive assessment of the patient’s condition is crucial for achieving the best possible outcomes.
2. Physical Therapy:
- Focus on improving strength, flexibility, balance, and mobility.
- Use exercises, gait training, and assistive devices to enhance functional abilities.
- Addressing pain management and preventing complications like pressure sores is vital as it significantly enhances the patient’s quality of life.
3. Occupational Therapy:
- Help patients regain independence in daily activities (e.g., dressing, grooming, cooking).
- Provide adaptive techniques and assistive devices.
- Address upper limb function and fine motor skills.
4. Speech-Language Pathology:
- Assist with communication difficulties (if applicable).
- Address swallowing issues (dysphagia) and provide strategies for safe eating.
5. Psychosocial Support:
Paralysis can be emotionally challenging. It’s crucial to provide counselling and support to patients and their families, acknowledging the emotional toll of the condition. By offering this support, we can help them navigate the psychological aspects of paralysis and foster a sense of understanding and empathy.
We can also encourage social participation and community integration. By doing so, we can help patients feel included and part of a larger community, fostering a sense of belonging and social support.
6. Nutrition and Dietetics:

- Ensure proper nutrition to support healing and prevent complications.
- Address any specific dietary needs related to paralysis.
Assistive Devices and Home Modifications:
- Evaluate the need for mobility aids (wheelchairs, walkers, canes).
- Modify the home environment for accessibility (ramps, grab bars, widened doorways).
Collaboration with Medical Professionals:
- Work closely with neurologists, orthopaedic surgeons, and other specialists.
Rehabilitation Technology for speedy and predictive recovery
Using appropriate and prescribed rehabilitation technology for patients leads to faster and more predictable recovery.
Wearable Sensors and IMUs:
- Wearable sensors and inertial measurement units (IMUs) capture movement autonomously and continuously.
- These technologies provide granular insights into movement dysfunction, helping professionals tailor personalised treatment approaches.
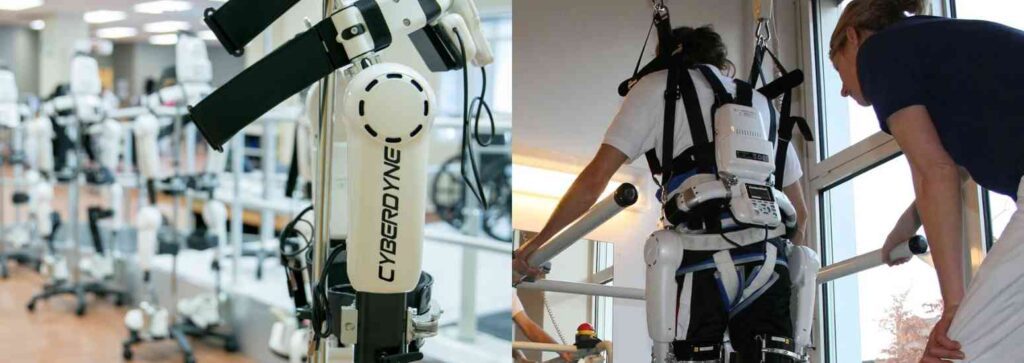
Robotic Devices for paralysis rehabilitation:
- Robot-assisted therapies aid in limb rehabilitation.
- They offer repetitive, precise movements to improve motor skills and regain function. Example: Cyberdyne – This neurorehab robotics helps the patients move their paretic or paralysed in faster and predictive recovery.
Virtual Reality treatment for Paralysis:
- VR environments engage patients in interactive exercises.
- This advanced rehabilitation technology enhance motivation, simulate real-world scenarios, and promote functional recovery.
Gamification:
- Gamified rehabilitation apps turn exercises into enjoyable activities.
- Patients stay motivated, leading to better adherence and faster recovery.
Neuroplasticity-Based Approaches:
- Leveraging the brain and spinal cord’s neuroplasticity, patients establish new neural pathways.
- This helps relearn motor skills and regain independence.
To know more about Paralysis Rehabilitation with advanced technologies and specialised technology-enabled treatment such as Cyberdyne, VIBRAMOOV and RECOVERIX, please connect with info@rehabmodalities.com or Visit our page
Source Reference:
Source 1 – Fox, M. H., Krahn, G. L., Sinclair, L. B., & Cahill, A. (2015). Using the international classification of functioning, disability and health to expand understanding of paralysis in the United States through improved surveillance. Disability and Health Journal.
Source 2 – Headache Treatment – Dr. Mohan Krishna Narasimha Kumar Jonnalagadda.



